The Weight Loss Drug Industrial Complex
A Deep Dive into Pharmaceutical Solutions
In our modern world, obesity and chronic illness have become the norm.
We're told to follow government guidelines, take our medications, and trust the system.
But what if this system is broken? What if the very civilization we've built is what's making us sick?
Today, let's take a look at the weight loss drugs that have been marketed as solutions to our health crises.
From the latest GLP-1 agonists to older amphetamine derivatives, we'll explore how they work, their efficacy, and whether they're truly helping us become healthier or just masking the symptoms of a deeper problem.
What started as just a curiosity and what I thought would be a small post has turned into an absolutely ginormous, comprehensive set of research.
Am I surprised? Not really. In the US, we spend $90B/year trying to lose weight. 45M Americans start a new diet every single year.
That does mean that somehow this post has turned out to be quite the textbook, much like my last one.
The Drugs
Semaglutide (Wegovy, Ozempic)
History: Developed by Novo Nordisk, approved for diabetes (Ozempic, 2017) and obesity (Wegovy, 2021).
Mechanism: GLP-1 receptor agonist. Mimics the GLP-1 hormone to increase satiety and slow gastric emptying.
Efficacy: Approximately 12-15% total body weight loss.
Cost: $997-$1,850/month.
Status: Approved for chronic use.
Adverse Effects: Nausea, vomiting, diarrhea, rare pancreatitis.
Semaglutide is the darling of the weight loss drug world right now, promising significant weight loss with just a weekly injection. But at nearly $2,000 a month (US, Branded, uninsured cost), it's not exactly accessible to everyone. And while it might help you lose weight, is it really addressing the root causes of obesity, or just another quick fix in a society that's addicted to instant gratification?
I've watched several videos of celebrity doctors try to explain how these drugs work. Every single one is different.
There are things that we clearly know - it slows down digestion, it increases satiety in your brain and increases your insulin response.
But there are things that we still don't understand, like why it will reduce impulsive shopping behavior, it reduces alcohol cravings, and increases fertility.
This doesn't cure any of the underlying drivers of obesity or weight gain, and therefore, most people come off it within a year, and most people regain a serious amount of weight after coming off.
Tirzepatide (Zepbound, Mounjaro)
History: Developed by Eli Lilly, approved for diabetes (Mounjaro, 2022) and obesity (Zepbound, 2023).
Mechanism: Dual GLP-1 and GIP receptor agonist. Enhances satiety and may boost metabolism.
Efficacy: Up to 18-21% body weight loss.
Cost: Approximately $1,000-$1,500/month.
Status: Approved for chronic use.
Adverse Effects: Gastrointestinal upset, rare thyroid tumors, pancreatitis.
Tirzepatide is even more effective than Semaglutide, with some patients losing up to 21% of their body weight.
It has similar unknowns to Semaglutide, but Is known for having less side effects.
Liraglutide (Saxenda)
History: Novo Nordisk, approved for diabetes (Victoza, 2010) and obesity (Saxenda, 2014).
Mechanism: GLP-1 receptor agonist. Increases satiety and slows gastric emptying.
Efficacy: Approximately 4-6% weight loss.
Cost: Approximately $1,300/month.
Status: Approved for chronic use.
Adverse Effects: Nausea, vomiting, pancreatitis.
Liraglutide has been around longer and is less effective than its newer counterparts. With only 4-6% weight loss, it's hard to justify the cost and side effects for many people.
Phentermine/Topiramate (Qsymia)
History: Vivus, approved 2012.
Mechanism: Phentermine suppresses appetite; Topiramate reduces food cravings.
Efficacy: 8-10% weight loss.
Cost: Approximately $100-$200/month.
Status: Approved for chronic use.
Adverse Effects: Insomnia, cognitive effects, dry mouth, teratogenicity.
Qsymia combines two drugs to achieve moderate weight loss. It's cheaper than the GLP-1 agonists, but the side effects, especially cognitive issues, might not be worth it for some.
Naltrexone/Bupropion (Contrave)
History: Orexigen, approved 2014.
Mechanism: Bupropion reduces cravings; Naltrexone reduces reward-driven eating.
Efficacy: Approximately 5% weight loss.
Cost: Approximately $99/month.
Status: Approved for chronic use.
Adverse Effects: Nausea, headache, increased blood pressure, risk of seizures.
With only 5% weight loss, Contrave is one of the least effective options. Its affordability is a plus, but the side effects, including seizure risk, are concerning.
Despite the efficacy during treatment, there is a notable gap in published research specifically addressing weight regain after discontinuing naltrexone for weight loss.
The American Academy of Family Physicians (AAFP) noted in 2015 that "it is unknown if weight gain occurs after stopping the medication," indicating a lack of long-term follow-up data at that time.
Orlistat (Xenical, Alli)
History: Roche (Xenical, 1999), GSK (Alli, OTC, 2007).
Mechanism: Lipase inhibitor; blocks fat absorption.
Efficacy: 3-5% weight loss.
Cost: $30-$60/month (OTC).
Status: Approved for chronic use.
Adverse Effects: Oily stools, diarrhea, fat-soluble vitamin deficiency.
Orlistat is available over the counter and is relatively cheap, but its side effects are notoriously unpleasant, and the weight loss is minimal.
If you block fat absorption in your body, it comes out in your poop, and this one is renowned for making people leak poop into their underwear.
Phentermine (Adipex-P, Lomaira)
History: Approved 1959, oldest prescription weight loss drug.
Mechanism: Sympathomimetic amine; suppresses appetite.
Efficacy: 5-10% weight loss (short-term use).
Cost: $20-$50/month.
Status: Approved for short-term use.
Adverse Effects: Insomnia, hypertension, tachycardia, abuse potential.
Phentermine is dirt cheap and has been around for decades, but it's only approved for short-term use due to its side effects and abuse potential.
I have read some conspiracy theories around how it was flagged for pulling and how faulty the studies were that said it was unhealthy.
Diethylpropion (Tenuate)
History: Approved 1959, similar to phentermine.
Mechanism: Sympathomimetic amine; suppresses appetite.
Efficacy: Approximately 10% weight loss (short-term use).
Cost: Varies.
Status: Approved for short-term use.
Adverse Effects: Similar to phentermine.
Diethylpropion is another old-school appetite suppressant, offering decent short-term results but with the same risks as Phentermine.
Benzphetamine (Didrex, Regimex)
History: Approved 1960s, amphetamine derivative.
Mechanism: Sympathomimetic amine; suppresses appetite.
Efficacy: Approximately 5-10% weight loss (short-term use).
Cost: Varies.
Status: Approved for short-term use.
Adverse Effects: Similar to phentermine.
Benzphetamine is less commonly used but follows the same pattern as other amphetamine derivatives: moderate efficacy with significant risks.
Phendimetrazine (Bontril, Melfiat)
History: Approved 1959, amphetamine derivative.
Mechanism: Sympathomimetic amine; suppresses appetite.
Efficacy: Approximately 5-10% weight loss (short-term use).
Cost: Varies.
Status: Approved for short-term use.
Adverse Effects: Similar to phentermine.
Phendimetrazine is another in the long line of amphetamine-like drugs, with similar benefits and drawbacks.
Methamphetamine (Desoxyn)
History: Approved for ADHD, also for short-term obesity treatment.
Mechanism: Potent CNS stimulant; suppresses appetite, increases metabolism.
Efficacy: Approximately 5-10% weight loss (short-term use).
Cost: Varies.
Status: Approved for short-term use, rarely prescribed due to abuse risk.
Adverse Effects: High abuse risk, cardiovascular and psychiatric effects.
Methamphetamine for weight loss? In what world is this a good idea? The risks far outweigh any potential benefits.
Lorcaserin (Belviq, withdrawn)
History: Eisai, approved 2012, withdrawn 2020 (cancer risk).
Mechanism: 5-HT2C serotonin receptor agonist; increases satiety.
Efficacy: Approximately 3-4% weight loss.
Status: Withdrawn.
Adverse Effects: Headache, dizziness, increased cancer risk.
Lorcaserin's withdrawal due to cancer risk highlights the potential dangers of these drugs, even after initial approval.
Sibutramine (Meridia, withdrawn)
History: Abbott, approved 1997, withdrawn 2010 (cardiovascular risk).
Mechanism: Serotonin-norepinephrine reuptake inhibitor; increases satiety, slightly increases metabolism.
Efficacy: Approximately 5% weight loss.
Status: Withdrawn.
Adverse Effects: Hypertension, heart attack, stroke.
Sibutramine's cardiovascular risks led to its withdrawal, a reminder that weight loss drugs can have serious consequences.
Rimonabant (Acomplia, withdrawn)
History: Sanofi, approved in Europe 2006, withdrawn 2008 (psychiatric risk).
Mechanism: CB1 cannabinoid receptor antagonist; reduces appetite and cravings.
Efficacy: Approximately 5% weight loss.
Status: Withdrawn.
Adverse Effects: Severe depression, suicide risk.
Rimonabant's psychiatric side effects were severe enough to pull it from the market, underscoring the mental health risks of some weight loss drugs.
Interestingly enough, if you dig into the psychiatric effects, Rimonabant is actually safer than gastric bypass. The mechanism by which this works is directly opposite to the way in which seed oils drive hunger, obesity, and cravings.
There are CB1 receptors in your brain and in your gut. When you can target the ones in your gut, you're gonna have a good time. When you target the ones in your brain, you're gonna have a bad time, which is what happened here.
In the next decade, we will see drugs that target CB1 receptors in the gut only come to market.
Setmelanotide (Imcivree)
History: For rare genetic obesity syndromes only.
Mechanism: MC4R agonist; increases satiety.
Manufacturer: Rhythm Pharmaceuticals.
Efficacy: Significant in rare disorders.
Status: Approved for rare genetic obesity.
Adverse Effects: Injection site reactions, hyperpigmentation.
Setmelanotide is a niche drug, effective for specific genetic conditions but not broadly applicable.
Plenity (Gelesis100)
History: FDA approved 2019.
Mechanism: Oral hydrogel expands in stomach to promote fullness.
Efficacy: Approximately 2-3% weight loss.
Status: Approved for chronic use.
Adverse Effects: Bloating, gastrointestinal discomfort.
Plenity's non-pharmacological approach is intriguing, but its minimal efficacy limits its impact.
Effectively stuffing your stomach can be done by other supplements & food too. Doesn’t solve any underlying issues.
Pramlintide (Symlin)
History: Approved for diabetes, studied for obesity.
Mechanism: Amylin analog; increases satiety by slowing gastric emptying.
Efficacy: Approximately 3-6% weight loss.
Status: Not FDA-approved for obesity alone.
Adverse Effects: Nausea.
Pramlintide's use for weight loss is off-label, with modest results and limited approval.
Metformin (Glucophage)
History: Approved for diabetes, used off-label for weight loss.
Mechanism: Increases insulin sensitivity, may increase satiety via GLP-1.
Efficacy: Approximately 2-3% weight loss.
Status: Not FDA-approved for obesity alone.
Adverse Effects: Gastrointestinal upset, rare lactic acidosis.
Metformin is a common off-label choice, but its weight loss effects are minimal.
Thyroid Hormones (Levothyroxine, T3, NDT)
History: Used for hypothyroidism; sometimes abused for weight loss.
Mechanism: Increases basal metabolic rate.
Efficacy: Only effective in hypothyroid patients; dangerous in euthyroid.
Status: Not approved for obesity.
Adverse Effects: Arrhythmia, osteoporosis, muscle loss.
Using thyroid hormones for weight loss in healthy individuals is a risky and unapproved practice, although before any real weight loss drugs came to market it was prescribed for weight loss - typically confirming that rare weight gain was driven by hypothyroidism back in the day.
Experimental Compounds
Adipotide
Adipotide (also known as FTPP or Prohibitin-TP01) is a synthetic peptide that targets blood vessels supplying white adipose tissue, causing selective apoptosis (cell death) of fat cells by cutting off their blood supply. This leads to fat loss and improved metabolic markers.
In obese rhesus monkeys, daily subcutaneous injections of Adipotide resulted in significant, dose-dependent weight loss: up to 20% reduction in body weight, 17% reduction in BMI, and 14% reduction in abdominal circumference over several weeks
Fat loss was confirmed by DEXA and MRI scans, with up to 39% decrease in fat deposits. Improvements in insulin resistance and metabolic health were also observed.
Human trials have been put on hold as the drug destroys fat cells indiscriminately It appears that in humans, that includes attacking the fat in kidneys and damaging kidneys and also attacking the fat in their brains.
Oddly, this is still sold by experimental peptide companies on the internet. Reddit users have noted that they literally feel like their brains are rotting when they use it.
Retarutide
Retatrutide is a novel “triple agonist” that activates GLP-1, GIP, and glucagon receptors.
This combination reduces appetite, improves glucose metabolism, and increases energy expenditure, making it more comprehensive than previous drugs like semaglutide or tirzepatide.
In phase 2 clinical trials, participants lost up to 24.2% of their body weight after 48 weeks of weekly injections-among the highest results for any obesity drug to date.
Most side effects are mild and gastrointestinal (nausea, diarrhea).
You can buy this again online quite cheaply from experimental peptide companies.
Users who switch to this from Ozempic report that the side effects they experience are way lower.
I would expect that on a long enough timeline, we'll see users that come off of this drug rebound the weight gain as it doesn't solve any underlying issues.
MOTS-C
MOTS-C is a mitochondrial-derived peptide that acts as an “exercise mimetic,” improving mitochondrial function, enhancing fatty acid metabolism, and increasing insulin sensitivity.
It was originally discovered when they were trying to find a peptide to give to elderly patients who moved into care homes and experienced sarcopenia.
It is being explored for its ability to prevent obesity, improve glucose regulation, and reduce inflammation.
In animal studies, MOTS-C prevented diet-induced obesity, reduced fat accumulation, and improved insulin sensitivity, especially in high-fat diet conditions.
Animal studies suggest a good safety profile, with benefits for metabolic health and no reported major adverse effects. More human data is needed.
Available from experimental peptide companies as an injection & nasal spray
DNP
DNP is a chemical that uncouples oxidative phosphorylation in mitochondria, causing the body to burn more energy as heat instead of storing it as fat. This dramatically increases metabolic rate and calorie burning
DNP can cause rapid weight loss (up to 1.5 kg per week) by increasing basal metabolic rate by 30–40%
DNP is extremely dangerous and potentially lethal. Side effects include uncontrolled hyperthermia (dangerously high body temperature), tachycardia, diaphoresis, and risk of death
The drug has a very narrow therapeutic window, and even small overdoses can be fatal. It was banned for human use in the 1930s after numerous deaths and cases of blindness due to cataracts.
DNP is not approved for weight loss and is considered unfit for human consumption by regulatory agencies worldwide.
Whilst I think that increasing metabolic rate should be the goal weight loss meds aspire to, DNP is acutely toxic to human mitochondria which totally defeats the point.
Supplements
Calocurb
Calocurb is a natural, plant-based appetite suppressant designed to support weight management by helping users feel full faster and reduce cravings. Its active ingredient is Amarasate®, a patented extract from New Zealand-grown bitter hops.
Calocurb works by stimulating the release of GLP-1, CCK, and PYY-gut hormones that signal satiety to the brain-helping reduce hunger by 30%, cravings by 40%, and calorie intake by 18% within an hour of use, according to clinical trials.
The reason I even know about this one is because Ben Greenfield seems to promote it all the time on his podcast. And that's where it's almost a bit uneasy because I generally find with anything in the weight loss space if it actually works, it will pass a bullshit detector. By that, I mean people will be posting about it on Reddit etc.
The amazon reviews aren’t great and it’s kinda expensive at $80 for about a 20 day supply.
Glucomannan
Glucomannan is a water-soluble dietary fiber derived from the root of the konjac plant. It is often used as a weight loss supplement due to its ability to absorb water and expand in the stomach, promoting a feeling of fullness and reducing calorie intake.
One study found no significant difference in weight loss compared to placebo after eight weeks, though other studies report small reductions in body weight (about 1.5–2.2 kg over several weeks).
Minor side effects: bloating, diarrhea, flatulence, abdominal discomfort.
Back to basics with this one - fill up your stomach = eat less
It’s $17 for 180 capsules and the Amazon reviews are much more positive.
T2 Thyroid
T2 is a naturally occurring thyroid hormone metabolite, distinct from the more commonly prescribed T4 (thyroxine) and T3 (triiodothyronine). T2 is gaining attention for its potential to boost metabolism and aid weight loss, particularly in thyroid patients.
Increases basal metabolic rate by enhancing mitochondrial activity, leading to higher energy expenditure at rest.
Promotes the browning of white fat, increasing thermogenesis and fat burning.
Limited human data: One study reported a 4% reduction in body weight over several weeks in people with normal thyroid function.
T2 is available over the counter in some supplement forms, unlike T3 and T4, which require a prescription.
Popular in bodybuilding circles because it doesn’t suppress T3 or T4
Like calocurb - I’m a bit meh on this. Where are the raving fans?
I know a few people who have tried DNP (idiots) but no one who has tried T2.
Physical and Surgical Interventions
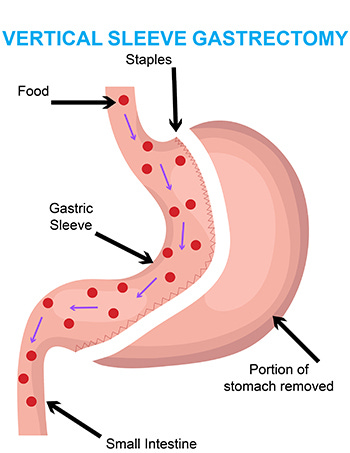
Sleeve Gastrectomy
Mechanism: Removes 80% of stomach, reduces ghrelin, increases satiety.
Efficacy: 20-25% total body weight loss.
Risks: Leak, reflux, nutrient deficiency.
Sleeve gastrectomy is highly effective but invasive, with lifelong nutritional implications. Many users report initial rapid weight loss, followed by weight regain. It’s almost as if losing weight by restricting calories permanently doesn’t work?
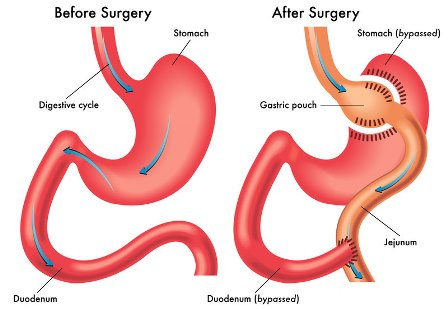
Roux-en-Y Gastric Bypass
Mechanism: Small stomach pouch, bypasses part of intestine; increases satiety and alters metabolism.
Efficacy: 25-35% total body weight loss.
Risks: Dumping syndrome, ulcers, malabsorption.
Gastric bypass offers dramatic results but comes with significant risks and lifestyle changes.
Interestingly enough this works similar to Rimonabant in that food is directed around your CB1 receptors and as such patients see the same benefits.
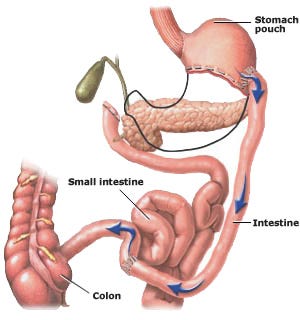
Biliopancreatic Diversion with Duodenal Switch
Mechanism: Combines sleeve and intestinal bypass; strong effect on satiety and metabolism.
Efficacy: 30-40% total body weight loss.
Risks: Severe malnutrition, diarrhea.
This procedure is the most effective but also the most risky, with severe potential complications.
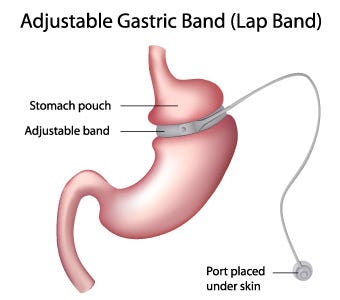
Adjustable Gastric Banding
Mechanism: Band restricts stomach size, increases satiety.
Efficacy: 10-20% total body weight loss.
Risks: Band slippage, erosion, less effective long-term.
Gastric banding is less invasive but has fallen out of favor due to lower long-term efficacy.
ObeEnd (Wristband)
Mechanism: Neuromodulation to reduce appetite; claims to increase brown fat.
Efficacy: Modest (4-8% reported).
Risks: Skin irritation, unproven long-term safety.
The wristband's claims are intriguing but lack robust evidence, making it a questionable option.
Quite honestly I was shocked that I had never heard of this when I found the website advertising the product. In fact, I actually emailed them to ask them if what they were selling was real. No response so far.
It's effectively a Fitbit with a little electrode that shocks you into not being hungry.
Conclusion
As we've seen, there's no shortage of weight loss drugs and interventions on the market, each with its own promises and pitfalls. From expensive injections that mimic hormones to surgical procedures that alter our digestive systems, these solutions reflect our obsession with quick fixes and technological interventions and that the market is willing to respond.
But are they truly making us healthier, or are they just symptoms of a deeper malaise?
Perhaps it's time to question whether these "solutions" are part of the problem.
Maybe, just maybe, the path to true health lies not in more civilization, but in becoming a little more uncivilized, returning to natural rhythms, eating whole foods, moving our bodies as nature intended, and listening to our innate wisdom rather than relying on pills and procedures.
After all, if civilization is making us sick, maybe it's time to become uncivilized.







It is time to rely less on drugs, and more on, effective healthy ways! Such as boosting happiness!
https://drjaneforhappiness.substack.com/p/the-happy-ways-of-weight-loss?r=31zx1q&utm_campaign=post&utm_medium=web&showWelcomeOnShare=false
I had access to mazindol years back and I liked it. DNP wasn’t my finest decision and I didn’t loose much weight for the nightmare that week was. I tired some of the tanning/ weight loss peptides but I’m covered in moles and yea they get dark, even ones I don’t normally see.