Beyond the Seed Oil Wars: A Clear-Eyed Look at How it Works & What the Science Actually Says
A response to some X clickbait
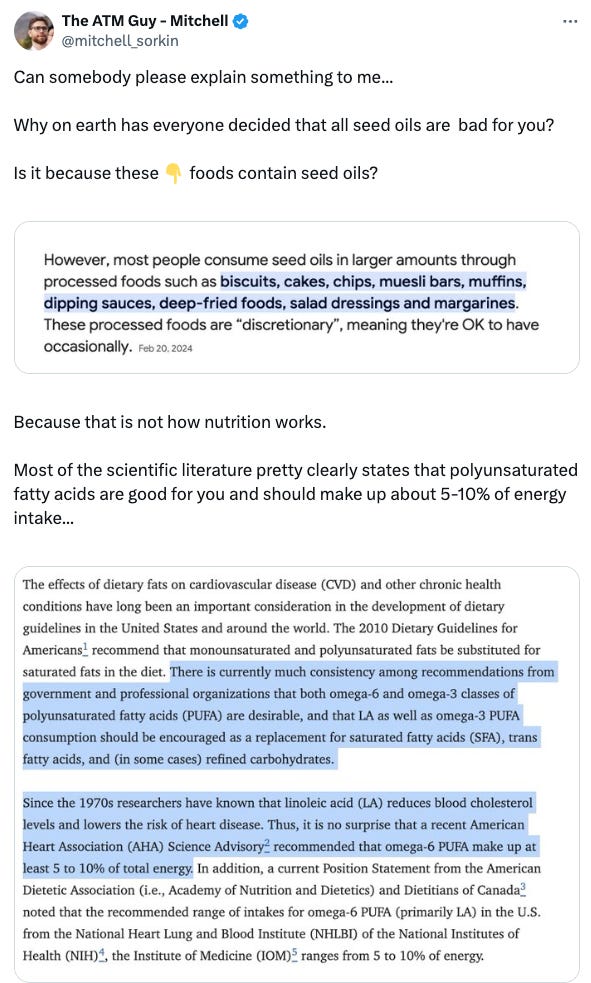
The Xeet below from the ATM Guy (12k followers on X) made its way into my timeline and every response was totally braindead. The tweet itself hit a nerve with me.
Saying these bad foods contain this thing thus the thing is bad, is not in fact the argument against seed oils, and actually biscuits, cakes, and dressings are mostly inert if made with naturally occurring fats.
Then to mention the lipid heart hypothesis - jeez this was such a bad take.
I replied with a comprehensive explanation of the key devil in seed oils - linoleic acid - an Omega 6 pufa and the nuances in how to interpret the whole body of evidence that implicates the causal relationship of dietary linoleic acid in modern chronic disease.
A comprehensive explanation that, I believe should be shared here rather than get lost into the twitterverse. Sadly, where the seed oil discourse fails is that this information exists in blogs and substacks (like this), and not on the website for a bona fide organization such as the American Heart Association. (I am working on this and hope to change said situation soon).
Introduction
Linoleic acid is a polyunsaturated Omega-6 fatty acid that plays a crucial role in human health.
It is considered an essential fatty acid because the human body cannot synthesize it; it must be obtained through diet.
Linoleic acid sources in the diet include nuts, seeds, and some meats, but primarily come from seed oils such as corn, soybean, sunflower, peanut, safflower, canola, rapeseed, grapeseed, cottonseed and rice bran oil.
While linoleic acid is vital for maintaining the structure of cell membranes and is involved in the production of signaling molecules, excessive consumption or an imbalanced consumption in relation to Omega-3 fats leads to negative health effects.
In a modern day context virtually every person living in the USA and other western nations is consuming linoleic acid at an imbalance to Omega-3 fats whilst also consuming excessive linoleic acid.
Metabolism of Linoleic Acid
Once ingested, linoleic acid undergoes metabolism in the body through a series of enzymatic reactions. Initially, linoleic acid is converted to gamma-linolenic acid (GLA) by the enzyme delta-6-desaturase.
GLA is then converted into dihomo-gamma-linolenic acid (DGLA), which can further be metabolized to form arachidonic acid (AA).
These metabolites, particularly arachidonic acid, are precursors to various eicosanoids, which are signaling molecules involved in inflammation and immune responses.
Peroxidation of Linoleic Acid
Lipid peroxidation, on the other hand, is a process that occurs under pathological conditions and involves the oxidative degradation of lipids.
Initiation: The reaction starts when a reactive oxygen species (ROS) or a free radical removes a hydrogen atom from a lipid, particularly from the unsaturated fatty acids in the lipid bilayer of cell membranes, creating a lipid radical.
Propagation: This lipid radical reacts with oxygen to form a lipid peroxyl radical, which can then react with another lipid molecule, creating a chain reaction of lipid radical formation and leading to widespread membrane damage.
Termination: The chain reaction ends when two radicals react together or are quenched by antioxidants.
The result of lipid peroxidation is the formation of a variety of breakdown products, including aldehydes like malondialdehyde (MDA) and 4-hydroxynonenal (4-HNE), which is toxic to cells and contributes to the pathology of various diseases, such as atherosclerosis, neurodegeneration, and cancer.
It is critical to understand that 4-HNE can create pathological oxidative stress such that the ingestion of linoleic acid creates a peroxidation cascade that is self fulfilling.
By many accounts the peroxidation of linoleic acid and its breakdown products in a western diet context, is the primary source of oxidative stress on the body.
Negative Effects of Consumption
1. Inflammation: A high intake of Omega-6 fatty acids, namely linoleic acid, relative to Omega-3 fatty acids, promotes inflammation in the body.
2. Oxidative Stress: Linoleic acid is more prone to oxidation than saturated or monounsaturated fats. The oxidation products of linoleic acid are the main driver of oxidative stress in the body, and cause cellular damage.
3. Unstable Cell Membranes: The incorporation of linoleic acid into human cell membranes creates inherently unstable cells. For example, the current level of consumption is such that linoleic acid levels in LDL cholesterol are artificially higher and as such these LDL particles are now more prone to oxidation than historically normal (LDL particles require oxidation to become atherosclerotic).
Understanding The Science Behind Linoleic Acid
Understanding the harmful effects of linoleic acid requires not just reviewing isolated studies, but a comprehensive synthesis of all available evidence across different animal models (including humans) and timelines.
Without this holistic approach, it’s easy to cherry-pick short-term studies to dismiss the long-term risks.
The ongoing debate over saturated fats (SFAs), polyunsaturated fats (PUFAs), and seed oils will never reach a conclusion unless there is a recognition of the need to integrate animal studies with both short-term and long-term human trials.
Critics often point to trials lasting no more than 12 weeks to argue against the findings from animal research, while ignoring pivotal long-term studies, such as the 8-year LA Veterans Administration Hospital Study.
They overlook mechanisms and instead treat the observed effects in short-term trials as standalone facts, missing the larger picture that understanding these mechanisms is essential to contextualizing the results.
To synthesize the evidence effectively, we must consider the following mechanisms:
1. Ethanol Metabolism and Fatty Liver: Ethanol’s metabolism via CYP2E1 generates reactive oxygen species (ROS), damaging ApoB and preventing the export of hepatic triglycerides.
2. Choline and ApoB Lipidation: In non-alcoholic models, choline deficiency impairs the lipidation of ApoB with phosphatidylcholine, a critical step in preventing fatty liver.
3. Nutrient Impact on Fatty Liver: Adequate protein, sulfur amino acids, and choline intake can eliminate fatty liver caused by alcohol, sugar, or fat.
4. Oxidation of PUFAs vs. SFAs: PUFAs oxidize more rapidly than SFAs, increasing the choline requirement for exporting SFAs from the liver.
5. Liver Fat and NASH Progression: In non-alcoholic models, SFAs worsen liver fat compared to PUFAs, but PUFAs accelerate progression to non-alcoholic steatohepatitis (NASH) due to oxidative damage, which is a more critical factor in NASH than the SFA/choline ratio.
6. Alcoholic Models: In contrast, SFAs protect against liver fat in alcoholic models because oxidative damage to ApoB outweighs the importance of the SFA/choline ratio.
7. Human Trials: Short-term human trials mimic non-alcoholic animal models, with SFAs increasing liver fat and PUFAs reducing it.
8. Long-Term Effects: Over extended periods, PUFAs are predicted to exacerbate NASH progression, the true threat to liver health and longevity.
9. The LA Veterans Administration Study: This study revealed that the detrimental effects of PUFAs in humans become apparent only after more than 8 years.
In sum, to truly understand the risks associated with linoleic acid, it’s essential to grasp the full scope of studies and the underlying mechanisms, rather than relying on selective, short-term evidence.
He said he would get back to me